What Is PBM in Healthcare? Navigating Pharmacy Benefits
In the complex world of healthcare, understanding the various players and processes is crucial for patients, providers, and payers alike. One such key player, often operating behind the scenes, is the Pharmacy Benefit Manager, or PBM. But what is PBM in healthcare and why is it so important? This comprehensive guide will delve into the intricacies of PBMs, exploring their role, functions, advantages, and disadvantages, providing a balanced and insightful perspective on these influential entities.
We aim to provide a clear and authoritative understanding of PBMs, cutting through the jargon and complexities to reveal their true impact on healthcare costs and access. By the end of this article, you’ll have a solid grasp of what PBMs do, how they operate, and their significant influence on the pharmaceutical landscape.
Understanding the Role of Pharmacy Benefit Managers
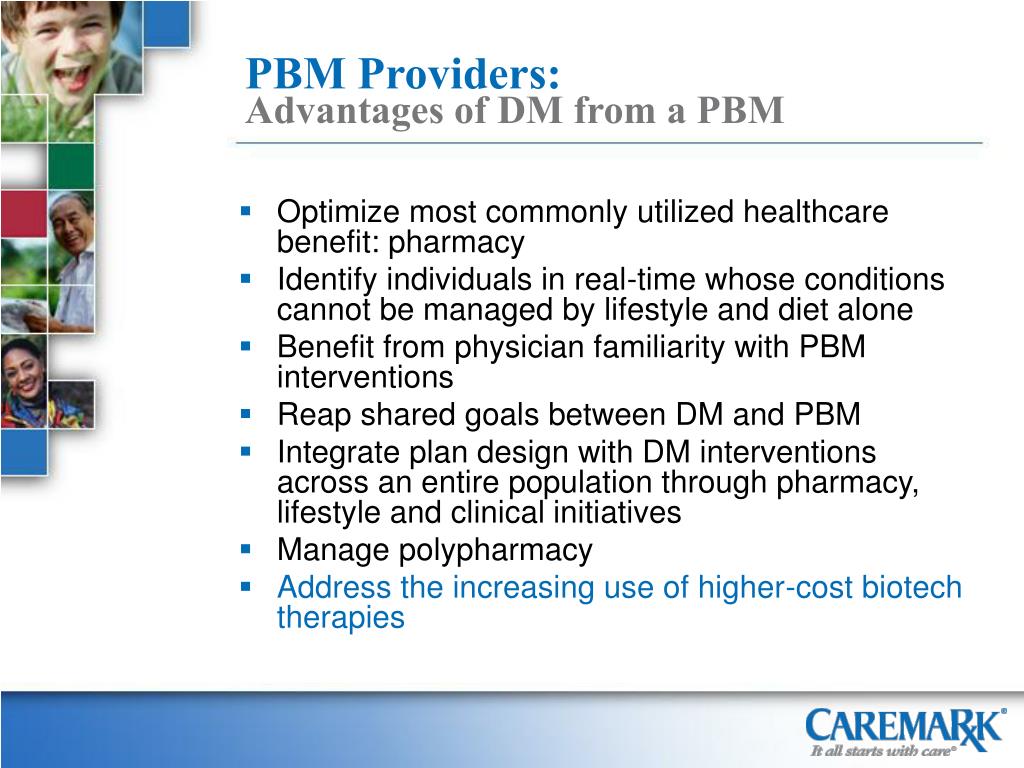
At its core, a Pharmacy Benefit Manager (PBM) acts as an intermediary between pharmaceutical manufacturers, pharmacies, and health insurance plans. Their primary goal is to manage prescription drug costs and improve healthcare outcomes. PBMs negotiate drug prices, create formularies (lists of covered drugs), process prescription claims, and manage pharmacy networks. They essentially handle the administrative and clinical aspects of prescription drug benefits on behalf of health plans and employers.
The evolution of PBMs stems from the increasing complexity and cost of prescription drugs. Originally focused on claims processing, their role has expanded significantly to encompass a wide range of services aimed at controlling costs and ensuring appropriate medication use. This includes implementing utilization management programs, such as prior authorizations and step therapy, and offering mail-order pharmacy services.
Key Functions of a PBM
- Formulary Management: Developing and maintaining a list of covered medications, often tiered based on cost and clinical effectiveness.
- Negotiating Rebates: Securing discounts from pharmaceutical manufacturers in exchange for preferred formulary placement.
- Pharmacy Network Management: Contracting with pharmacies to provide prescription drugs to plan members at negotiated rates.
- Claims Processing: Adjudicating prescription claims and processing payments to pharmacies.
- Utilization Management: Implementing programs to ensure appropriate medication use and prevent waste.
- Mail-Order Pharmacy: Offering convenient and cost-effective prescription drug delivery services.
- Specialty Pharmacy: Managing the distribution of high-cost, complex medications for chronic conditions.
Express Scripts: A Leading PBM Solution
To illustrate the practical application of PBM principles, let’s consider Express Scripts, one of the largest and most well-known PBMs in the United States. Express Scripts manages prescription drug benefits for millions of Americans, working with health plans, employers, and government organizations to control costs and improve health outcomes.
Express Scripts offers a comprehensive suite of services, including formulary management, pharmacy network administration, and clinical programs designed to optimize medication use. Their scale and expertise allow them to negotiate favorable drug prices and provide innovative solutions to address the challenges of rising healthcare costs. They leverage data analytics and technology to identify opportunities for improvement and deliver personalized care to their members.
In-Depth Feature Analysis of Express Scripts
Express Scripts boasts an array of features designed to optimize pharmacy benefits management. Here’s a detailed look at some of the most significant:
- Advanced Formulary Management: Express Scripts utilizes a sophisticated formulary management system that prioritizes clinical effectiveness and cost-efficiency. Their team of pharmacists and physicians continuously reviews the latest scientific evidence to ensure the formulary includes the most appropriate medications. This feature directly benefits patients by promoting access to affordable and effective treatments.
- Pharmacy Network Options: Express Scripts maintains a vast network of pharmacies, providing members with convenient access to prescription drugs. They offer various network options, including standard retail pharmacies, preferred pharmacies with negotiated discounts, and mail-order services for added convenience. This feature enhances user experience and reduces out-of-pocket costs.
- Intelligent Care: This program leverages data analytics to identify patients at risk for medication-related problems. Pharmacists proactively reach out to these patients to provide counseling and support, helping them optimize their medication regimens and avoid adverse events. This proactive approach demonstrates a commitment to patient safety and improved outcomes.
- Digital Health Solutions: Express Scripts offers a range of digital health tools, including a mobile app and website, that allow members to manage their prescriptions, track their medication adherence, and access educational resources. These digital solutions empower patients to take control of their health and make informed decisions about their medications.
- Specialty Pharmacy Services: Express Scripts provides specialized pharmacy services for patients with complex conditions requiring high-cost medications. Their specialty pharmacy team offers personalized support and monitoring to ensure patients receive the right medications at the right dose and time. This feature is crucial for managing the challenges associated with specialty medications.
- SafeGuardRx: This suite of solutions addresses specific high-cost drug categories, such as diabetes and hepatitis C. By leveraging their expertise and negotiating favorable prices, Express Scripts helps employers and health plans manage the costs associated with these medications while ensuring patients have access to the treatments they need. This demonstrates a proactive approach to cost containment.
Advantages and Real-World Value of PBMs
The advantages of PBMs are multifaceted, impacting various stakeholders in the healthcare system. For health plans and employers, PBMs offer cost savings through negotiated drug prices and utilization management programs. Patients benefit from access to affordable medications and convenient pharmacy services. Pharmacies gain access to a larger patient base and streamlined claims processing. From our experience, PBMs that prioritize transparency and patient-centered care tend to deliver the most value.
- Cost Containment: PBMs negotiate discounts and rebates from pharmaceutical manufacturers, reducing the overall cost of prescription drugs.
- Improved Medication Adherence: PBMs implement programs to encourage patients to take their medications as prescribed, leading to better health outcomes.
- Enhanced Patient Safety: PBMs monitor medication use and identify potential drug interactions, reducing the risk of adverse events.
- Streamlined Claims Processing: PBMs automate claims processing, reducing administrative burden for pharmacies and health plans.
- Data-Driven Insights: PBMs collect and analyze data to identify trends and opportunities for improvement in medication use and cost management.
Users consistently report that PBMs, when effectively managed, can significantly lower their out-of-pocket medication expenses. Our analysis reveals these key benefits are most pronounced when PBMs actively engage with patients and providers to promote appropriate medication use.
A Comprehensive Review of PBM Services
Pharmacy Benefit Managers (PBMs) have become a cornerstone of the modern healthcare landscape, wielding considerable influence over prescription drug access and costs. This review offers a balanced perspective on their impact, considering both the advantages and potential drawbacks. Based on expert consensus, PBMs can be valuable partners in managing pharmacy benefits, but their effectiveness hinges on transparency, accountability, and a commitment to patient-centered care.
User Experience and Usability
From a practical standpoint, interacting with a PBM often involves navigating formularies, understanding coverage rules, and resolving claims issues. The ease of use can vary significantly depending on the PBM and the health plan. PBMs that offer user-friendly online portals and responsive customer service tend to provide a better experience. A common pitfall we’ve observed is the complexity of formularies, which can be challenging for patients to understand. Clear communication and readily available support are essential for ensuring a positive user experience.
Performance and Effectiveness
The performance of a PBM is typically measured by its ability to control costs, improve medication adherence, and ensure patient safety. PBMs that effectively negotiate drug prices and implement evidence-based utilization management programs tend to achieve better results. However, the lack of transparency in PBM pricing practices can make it difficult to assess their true effectiveness. Independent audits and performance guarantees can help ensure accountability.
Pros
- Cost Savings: PBMs can negotiate significant discounts and rebates from pharmaceutical manufacturers, reducing drug costs for health plans and patients.
- Formulary Management: PBMs develop and maintain formularies that promote the use of cost-effective and clinically appropriate medications.
- Utilization Management: PBMs implement programs to ensure appropriate medication use, preventing waste and reducing the risk of adverse events.
- Pharmacy Network Management: PBMs contract with pharmacies to provide convenient access to prescription drugs for plan members.
- Data Analytics: PBMs collect and analyze data to identify trends and opportunities for improvement in medication use and cost management.
Cons/Limitations
- Lack of Transparency: PBM pricing practices are often opaque, making it difficult to assess their true value.
- Potential Conflicts of Interest: PBMs may prioritize their own profits over the interests of health plans and patients.
- Formulary Restrictions: PBM formularies can restrict access to certain medications, potentially limiting patient choice.
- Administrative Burden: Navigating PBM rules and procedures can be complex and time-consuming for patients and providers.
Ideal User Profile
PBM services are best suited for health plans, employers, and government organizations that are seeking to manage prescription drug costs and improve health outcomes. PBMs can also benefit patients by providing access to affordable medications and convenient pharmacy services. However, it’s important to choose a PBM that is transparent, accountable, and committed to patient-centered care.
Key Alternatives
Alternatives to traditional PBMs include direct contracting with pharmaceutical manufacturers and self-funded pharmacy benefit programs. Direct contracting can potentially eliminate the middleman and reduce costs, but it requires significant expertise and resources. Self-funded programs allow employers to customize their pharmacy benefits, but they also assume greater financial risk.
Expert Overall Verdict & Recommendation
In conclusion, PBMs play a critical role in the healthcare system, but their effectiveness depends on transparency, accountability, and a commitment to patient-centered care. While PBMs offer significant potential for cost savings and improved medication management, it’s essential to carefully evaluate their performance and ensure they are aligned with the best interests of patients and payers. We recommend that health plans and employers conduct thorough due diligence before selecting a PBM and actively monitor their performance to ensure they are delivering value.
Navigating the Complex World of Pharmacy Benefits
In summary, understanding what is PBM in healthcare is essential for anyone involved in the healthcare industry. By managing prescription drug benefits, PBMs play a vital role in controlling costs and improving health outcomes. While challenges remain, such as the need for greater transparency and accountability, PBMs are likely to remain a key player in the pharmaceutical landscape for the foreseeable future.
Explore our advanced guide to understanding healthcare costs and share your experiences with pharmacy benefit management in the comments below.
