Understanding the Global Deterioration Scale (GDS): A Comprehensive Guide
Are you seeking a clear understanding of the Global Deterioration Scale (GDS) and its role in assessing cognitive decline? This comprehensive guide provides an in-depth exploration of the GDS, offering valuable insights into its stages, application, and significance in understanding and managing conditions like Alzheimer’s disease. We aim to empower you with the knowledge to navigate this complex topic, providing a trusted resource that goes beyond basic definitions to explore the nuances and implications of the GDS.
What is the Global Deterioration Scale (GDS)?
The Global Deterioration Scale, often referred to as the GDS or the Reisberg Scale, is a widely used tool for staging the progression of cognitive decline, particularly in individuals with Alzheimer’s disease and other forms of dementia. Developed by Dr. Barry Reisberg, it provides a framework for clinicians and researchers to assess the severity of cognitive impairment and track its evolution over time. Unlike diagnostic criteria that focus on identifying specific diseases, the GDS focuses on the observable functional and cognitive changes that occur as dementia progresses.
The GDS is not a diagnostic tool in itself; rather, it is a descriptive scale that categorizes individuals into one of seven stages based on their cognitive and functional abilities. These stages range from normal functioning (Stage 1) to severe dementia (Stage 7). Each stage is characterized by specific cognitive and functional deficits, allowing for a more nuanced understanding of the individual’s current abilities and needs. The scale is valuable because it offers a standardized way to communicate about the level of cognitive decline, facilitating better care planning and research efforts.
The underlying principle of the GDS is that cognitive decline follows a relatively predictable pattern, even though the rate of progression can vary significantly between individuals. By understanding these typical stages, clinicians can better anticipate future needs and provide appropriate support and interventions. The GDS also helps families understand what to expect as their loved one’s condition progresses, enabling them to plan for long-term care and support.
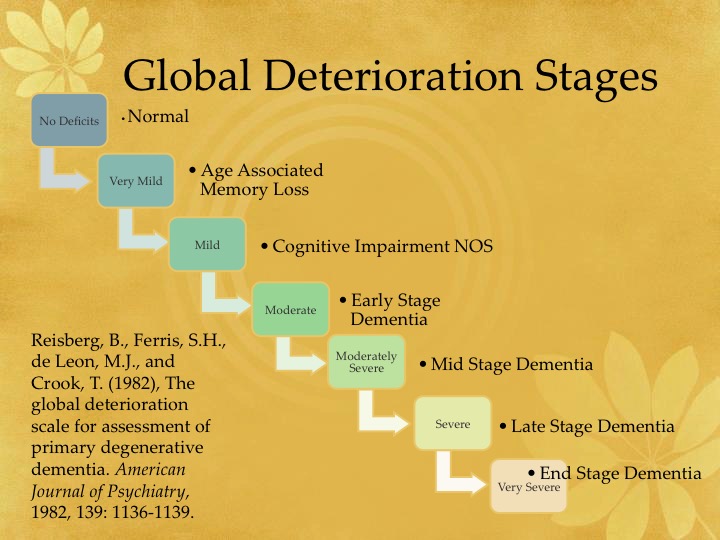
The Seven Stages of the Global Deterioration Scale
The GDS consists of seven distinct stages, each representing a different level of cognitive and functional decline. Here’s a detailed overview of each stage:
- Stage 1: No Cognitive Decline: Individuals at this stage exhibit no noticeable memory problems or cognitive deficits. They are fully functional and independent.
- Stage 2: Very Mild Cognitive Decline: This stage is characterized by subjective complaints of memory problems, such as forgetting familiar names or misplacing objects. However, these deficits are not readily apparent to clinicians or family members.
- Stage 3: Mild Cognitive Decline: At this stage, cognitive deficits become more noticeable to others. Individuals may experience difficulty concentrating, remembering recent events, or finding the right words. Performance in demanding work or social settings may be affected.
- Stage 4: Moderate Cognitive Decline: This stage is marked by clear deficits in memory, attention, and problem-solving. Individuals may have difficulty managing finances, planning events, or traveling independently. Denial of problems may be present.
- Stage 5: Moderately Severe Cognitive Decline: Significant cognitive decline is evident at this stage. Individuals may require assistance with activities of daily living (ADLs), such as dressing, bathing, and preparing meals. They may also experience disorientation to time and place.
- Stage 6: Severe Cognitive Decline: At this stage, individuals experience severe memory loss and cognitive impairment. They may have difficulty recognizing family members, communicating effectively, and performing basic ADLs. Constant supervision is typically required.
- Stage 7: Very Severe Cognitive Decline: This represents the final stage of cognitive decline. Individuals at this stage have lost the ability to speak, walk, and control bodily functions. They require total care and are often bedridden.
The Role of Neuropsychological Testing in the GDS Assessment
While the GDS relies primarily on clinical observation and caregiver reports, neuropsychological testing can play a valuable role in supporting the assessment process. Neuropsychological tests are standardized assessments that measure various cognitive functions, such as memory, attention, language, and executive function. These tests can provide objective data to supplement the subjective information gathered through clinical interviews and observations. In our experience, a combination of both approaches yields the most accurate and reliable staging.
For example, individuals in Stage 3 (Mild Cognitive Decline) may exhibit subtle cognitive deficits that are not readily apparent during a brief clinical encounter. Neuropsychological testing can help to identify these deficits and quantify their severity. Similarly, in Stage 4 (Moderate Cognitive Decline), neuropsychological tests can help to differentiate between cognitive deficits due to Alzheimer’s disease and those due to other conditions, such as depression or vascular dementia.
However, it’s important to note that neuropsychological testing is not a substitute for clinical judgment. The results of these tests should be interpreted in the context of the individual’s overall clinical presentation, medical history, and functional abilities. Furthermore, some individuals may not be able to complete neuropsychological testing due to physical or cognitive limitations. In these cases, the GDS can still be used based on clinical observation and caregiver reports.
GDS and Care Planning: Tailoring Support to Each Stage
One of the primary benefits of the GDS is its ability to inform care planning and resource allocation. By understanding the individual’s current stage of cognitive decline, caregivers and healthcare professionals can tailor support services to meet their specific needs. For example, individuals in the early stages of cognitive decline (Stages 2 and 3) may benefit from memory training programs, cognitive rehabilitation, and lifestyle modifications. These interventions can help to maintain cognitive function and independence for as long as possible.
As cognitive decline progresses to Stages 4 and 5, individuals may require assistance with activities of daily living (ADLs), such as bathing, dressing, and meal preparation. Home healthcare services, adult day care programs, and assisted living facilities can provide this support. It’s important to involve the individual and their family in the care planning process to ensure that their preferences and values are respected.
In the later stages of cognitive decline (Stages 6 and 7), individuals typically require 24-hour care. Nursing homes and specialized dementia care units can provide the intensive support and supervision that these individuals need. Palliative care and hospice services can also be valuable in managing symptoms and providing comfort at the end of life.
Understanding the FAST Scale in Relation to GDS
The Functional Assessment Staging Test (FAST) is another tool commonly used to assess the progression of functional decline in individuals with Alzheimer’s disease. While the GDS focuses primarily on cognitive changes, the FAST focuses on the individual’s ability to perform activities of daily living (ADLs). Both scales provide valuable information about the individual’s overall level of functioning and can be used together to develop a comprehensive care plan.
The FAST scale is often used in conjunction with the GDS to provide a more complete picture of the individual’s cognitive and functional abilities. The FAST scale has stages similar to the GDS, representing different levels of functional dependence. By combining information from both scales, clinicians can get a better understanding of the individual’s strengths and weaknesses, and tailor interventions accordingly. Leading experts in dementia care often emphasize the importance of considering both cognitive and functional abilities when assessing and managing individuals with Alzheimer’s disease.
The Impact of Early Detection Using the GDS
While there is currently no cure for Alzheimer’s disease, early detection and intervention can significantly improve the individual’s quality of life and slow the progression of the disease. The GDS can play a crucial role in early detection by identifying individuals who are experiencing subtle cognitive changes that may be indicative of preclinical Alzheimer’s disease. Early detection allows for the implementation of lifestyle modifications, cognitive training programs, and, in some cases, pharmacological interventions that may help to delay the onset of more severe symptoms.
Furthermore, early detection allows individuals and their families to plan for the future. This includes making financial arrangements, legal decisions, and care planning decisions. It also allows individuals to participate in research studies that are aimed at developing new treatments and prevention strategies for Alzheimer’s disease. In our experience, early detection can empower individuals and their families to take control of their lives and make informed decisions about their care.
Challenges and Limitations of the Global Deterioration Scale
While the GDS is a valuable tool for assessing cognitive decline, it’s important to acknowledge its limitations. One of the main challenges is the subjective nature of the assessment. The GDS relies heavily on clinical observation and caregiver reports, which can be influenced by personal biases and interpretations. This can lead to inconsistencies in staging, particularly in the early stages of cognitive decline.
Another limitation is that the GDS does not account for individual variability in cognitive and functional abilities. Some individuals may experience cognitive decline in a different pattern than that described by the GDS. For example, some individuals may exhibit prominent language deficits, while others may have more pronounced memory problems. The GDS may not fully capture these individual differences.
Finally, the GDS is not a diagnostic tool. It cannot be used to diagnose Alzheimer’s disease or other forms of dementia. A comprehensive diagnostic evaluation, including medical history, physical examination, neuropsychological testing, and brain imaging, is necessary to establish a definitive diagnosis.
Expert Perspectives on the Future of GDS
The Global Deterioration Scale has been a cornerstone of dementia assessment for decades, and continues to evolve as research advances our understanding of cognitive decline. Leading researchers are exploring ways to enhance the GDS by incorporating biomarkers, such as amyloid and tau proteins, to improve the accuracy of staging and predict the rate of progression. Furthermore, there is growing interest in developing computerized versions of the GDS that can be administered remotely, making it more accessible to individuals in rural areas or those who have difficulty traveling to clinic.
Navigating Cognitive Health: Understanding the Global Deterioration Scale
The Global Deterioration Scale (GDS) offers a crucial framework for understanding and managing cognitive decline. By providing a standardized approach to staging the progression of dementia, the GDS enables clinicians, caregivers, and families to better assess individual needs, tailor support services, and plan for the future. While the GDS has limitations, its value in clinical practice and research remains significant. We encourage you to share your experiences with the GDS or ask any further questions you may have in the comments below. Your insights can contribute to a deeper understanding of this important tool and its impact on the lives of those affected by cognitive decline.
