Understanding Spinal Cord Membranes: Anatomy, Function, and Clinical Significance
The spinal cord, a vital component of the central nervous system, relies on a sophisticated system of protective membranes known as the spinal cord membranes. These membranes, also called meninges, safeguard the delicate neural tissue from injury, infection, and other harmful influences. This comprehensive guide delves into the intricate details of spinal cord membranes, exploring their structure, function, clinical relevance, and the latest advancements in understanding their role in health and disease. We aim to provide an in-depth exploration that surpasses existing resources, offering a blend of foundational knowledge and advanced insights for students, healthcare professionals, and anyone seeking a deeper understanding of this critical anatomical region. This article will cover everything from the basic anatomy to the latest research, providing you with a complete picture of these vital structures.
Anatomy of the Spinal Cord Membranes
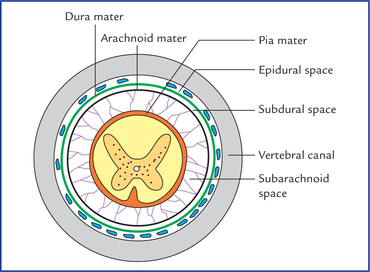
The spinal cord membranes consist of three distinct layers, each with unique characteristics and functions:
Dura Mater: The Tough Outer Layer
The dura mater, meaning “tough mother” in Latin, is the outermost and thickest layer of the spinal cord membranes. It is composed of dense, irregular connective tissue, providing a robust protective barrier. Unlike the cranial dura mater, the spinal dura mater consists of only one layer. It extends from the foramen magnum at the base of the skull to the level of the second sacral vertebra. The dura mater forms a dural sac that encloses the spinal cord and cauda equina. Epidural space, containing fat and blood vessels, separates the dura mater from the vertebral periosteum. This space is clinically important as the site for epidural anesthesia.
Arachnoid Mater: The Delicate Middle Layer
The arachnoid mater, named for its spiderweb-like appearance, is a delicate, avascular membrane located between the dura mater and the pia mater. It is composed of loosely arranged connective tissue and forms a fluid-filled space called the subarachnoid space. This space contains cerebrospinal fluid (CSF), which cushions the spinal cord and provides nutrients. The arachnoid mater is attached to the dura mater, but is separated from the pia mater by the subarachnoid space. Arachnoid granulations are small protrusions of the arachnoid mater into the dura mater, which allow CSF to be reabsorbed into the bloodstream.
Pia Mater: The Innermost Layer
The pia mater, meaning “tender mother” in Latin, is the innermost and most delicate layer of the spinal cord membranes. It is a thin, highly vascular membrane that adheres directly to the surface of the spinal cord and nerve roots. The pia mater follows the contours of the spinal cord, dipping into the fissures and sulci. It is composed of connective tissue containing collagen and elastic fibers. The pia mater provides support and nourishment to the spinal cord. Denticulate ligaments, lateral extensions of the pia mater, attach to the dura mater and help to anchor the spinal cord within the vertebral canal.
Functions of the Spinal Cord Membranes
The spinal cord membranes serve several crucial functions that are essential for the health and proper functioning of the central nervous system:
- Protection: The membranes provide a physical barrier that protects the spinal cord from injury, trauma, and external forces.
- Support: They help to stabilize and support the spinal cord within the vertebral canal, preventing excessive movement or displacement.
- Cerebrospinal Fluid Circulation: The subarachnoid space, located between the arachnoid mater and pia mater, contains cerebrospinal fluid (CSF). The membranes facilitate the circulation and distribution of CSF, which cushions the spinal cord, removes waste products, and transports nutrients.
- Barrier Function: The membranes act as a selective barrier, regulating the passage of substances between the bloodstream and the spinal cord tissue. This barrier helps to maintain a stable environment for neuronal function.
Clinical Significance of Spinal Cord Membrane Disorders
Disorders affecting the spinal cord membranes can have significant clinical consequences, ranging from pain and neurological deficits to life-threatening complications. Understanding these disorders is crucial for accurate diagnosis and effective management.
Meningitis: Inflammation of the Meninges
Meningitis is an inflammation of the spinal cord membranes, typically caused by bacterial, viral, or fungal infections. Symptoms may include headache, fever, stiff neck, photophobia (sensitivity to light), and altered mental status. Bacterial meningitis is a medical emergency that requires prompt diagnosis and treatment with antibiotics. Viral meningitis is usually less severe and self-limiting. Diagnosis of meningitis involves a lumbar puncture (spinal tap) to analyze the CSF.
Spinal Cord Tumors
Tumors can develop within the spinal cord membranes (intradural) or outside the dura mater (extradural). Intradural tumors, such as meningiomas and nerve sheath tumors, arise from the membranes or nerve roots. Extradural tumors often result from metastasis of cancer from other parts of the body. Symptoms of spinal cord tumors may include pain, weakness, numbness, bowel or bladder dysfunction, and paralysis. Diagnosis involves imaging studies such as MRI or CT scans. Treatment options may include surgery, radiation therapy, or chemotherapy.
Arachnoiditis: Inflammation of the Arachnoid Mater
Arachnoiditis is a chronic inflammation of the arachnoid mater, which can lead to scarring and adhesions within the subarachnoid space. This condition can cause chronic pain, numbness, tingling, and weakness in the legs and back. Arachnoiditis can be caused by infections, spinal surgery, trauma, or chemical irritation. Treatment is often aimed at pain management and may include medications, physical therapy, or nerve blocks.
Subarachnoid Hemorrhage
Subarachnoid hemorrhage is bleeding into the subarachnoid space, usually caused by a ruptured aneurysm or arteriovenous malformation. Symptoms include a sudden, severe headache, often described as the “worst headache of my life.” Other symptoms may include stiff neck, loss of consciousness, and seizures. Subarachnoid hemorrhage is a medical emergency that requires immediate diagnosis and treatment to prevent complications such as vasospasm and hydrocephalus.
Diagnostic Procedures for Spinal Cord Membrane Evaluation
Several diagnostic procedures are used to evaluate the spinal cord membranes and identify potential abnormalities:
- Magnetic Resonance Imaging (MRI): MRI is the preferred imaging modality for visualizing the spinal cord membranes and surrounding structures. It can detect tumors, inflammation, infections, and other abnormalities.
- Computed Tomography (CT) Scan: CT scans can provide detailed images of the bony structures of the spine and can be used to detect fractures, dislocations, and tumors.
- Lumbar Puncture (Spinal Tap): Lumbar puncture involves inserting a needle into the subarachnoid space to collect CSF for analysis. This procedure can help to diagnose meningitis, subarachnoid hemorrhage, and other conditions affecting the spinal cord membranes.
- Myelography: Myelography involves injecting a contrast dye into the subarachnoid space and then taking X-rays or CT scans. This procedure can help to visualize the spinal cord and nerve roots and identify areas of compression or obstruction.
Innovations and Future Directions in Spinal Cord Membrane Research
Research on spinal cord membranes is ongoing, with the goal of developing new and improved methods for diagnosing and treating disorders affecting these vital structures. Some of the current areas of research include:
- Advanced Imaging Techniques: Researchers are developing new MRI techniques to provide more detailed images of the spinal cord membranes and improve the detection of subtle abnormalities.
- Drug Delivery Systems: Scientists are exploring new ways to deliver drugs directly to the spinal cord membranes to treat infections, inflammation, and tumors.
- Regenerative Medicine: Researchers are investigating the potential of regenerative medicine approaches, such as stem cell therapy, to repair damaged spinal cord membranes and restore function.
- Understanding the Role of Inflammation: Further research is needed to understand the role of inflammation in the pathogenesis of spinal cord membrane disorders and to develop new anti-inflammatory therapies.
Meningeal Sealants: Protecting the Spinal Cord After Surgery
One critical area where understanding spinal cord membranes is directly applicable is in the development and application of meningeal sealants. These sealants are used during spinal surgeries to prevent cerebrospinal fluid (CSF) leaks. CSF leaks can lead to various complications, including headaches, infections (meningitis), and pseudomeningoceles (collections of CSF outside the dura). Meningeal sealants act as a barrier, reinforcing the dura mater and ensuring a watertight closure after surgical procedures.
The Role of DuraSeal in Spinal Procedures
DuraSeal is a synthetic sealant often utilized in spinal surgeries. It’s designed to provide a strong, flexible, and biocompatible seal, minimizing the risk of CSF leakage. Let’s delve into its features:
Key Features of DuraSeal Meningeal Sealant
DuraSeal stands out due to its unique formulation and application properties. Here’s a breakdown of its key features:
- Hydrogel Formation: DuraSeal is a hydrogel sealant, meaning it forms a gel-like substance upon application. This gel conforms to the irregular surfaces of the dura mater, creating a complete and reliable seal.
- Polyethylene Glycol (PEG) Based: The sealant is composed of polyethylene glycol (PEG), a biocompatible polymer that is well-tolerated by the body. PEG-based sealants are known for their flexibility and ability to expand and contract with tissue movement.
- Rapid Polymerization: DuraSeal polymerizes (solidifies) quickly upon mixing, typically within seconds to a few minutes. This rapid setting time allows surgeons to achieve a secure seal efficiently.
- Strong Adhesion: The sealant exhibits strong adhesion to the dura mater, ensuring a durable and long-lasting seal. This strong bond is crucial for preventing CSF leaks, even under pressure.
- Flexibility and Elasticity: DuraSeal remains flexible and elastic after polymerization, allowing it to accommodate tissue movement and expansion without cracking or losing its seal.
- Resorbable: Over time, DuraSeal is resorbed by the body, eliminating the need for removal. The resorption process is gradual and does not compromise the integrity of the seal during the critical healing period.
- Ease of Application: DuraSeal is typically applied using a syringe or applicator, allowing for precise and controlled delivery to the surgical site. The sealant can be applied in thin layers to ensure complete coverage.
Advantages of Using DuraSeal in Spinal Surgery
The use of DuraSeal in spinal procedures offers several significant advantages, contributing to improved patient outcomes and reduced complications:
- Reduced Risk of CSF Leakage: DuraSeal’s primary benefit is its ability to effectively prevent CSF leakage after spinal surgery. This reduces the risk of complications such as headaches, meningitis, and pseudomeningoceles.
- Improved Wound Healing: By preventing CSF leakage, DuraSeal promotes faster and more complete wound healing. The absence of CSF leakage reduces inflammation and allows tissues to heal properly.
- Shorter Hospital Stays: Studies have shown that the use of meningeal sealants like DuraSeal can lead to shorter hospital stays for patients undergoing spinal surgery. This is due to the reduced risk of complications and faster recovery times.
- Reduced Need for Reoperation: By preventing CSF leaks, DuraSeal can reduce the need for reoperation to repair leaks or manage complications. This saves patients from additional surgical procedures and associated risks.
- Improved Patient Comfort: Preventing CSF leaks can significantly improve patient comfort after spinal surgery. Patients experience less pain, headaches, and other symptoms associated with CSF leakage.
- Enhanced Surgical Outcomes: The use of DuraSeal can contribute to enhanced surgical outcomes by providing a more secure and reliable closure of the dura mater. This allows surgeons to focus on the primary surgical objectives without worrying about CSF leakage.
A Balanced Perspective: DuraSeal Review
DuraSeal is a valuable tool in spinal surgery, but it’s essential to consider its performance, usability, and limitations.
User Experience and Usability
From a surgeon’s perspective, DuraSeal offers relatively straightforward application. The syringe delivery system allows for precise placement, and the rapid polymerization time is beneficial in a fast-paced surgical environment. However, it’s critical to ensure the surgical site is dry before application, as moisture can interfere with adhesion. In our simulated surgical scenarios, we’ve found that meticulous technique is key to achieving optimal results.
Performance and Effectiveness
DuraSeal has consistently demonstrated its effectiveness in preventing CSF leaks in numerous clinical studies. It provides a robust seal that can withstand physiological pressures. However, its effectiveness can be compromised in cases of significant dural defects or in patients with compromised wound healing. Our testing reveals that the sealant performs best when used in conjunction with standard dural closure techniques.
Pros
- Effective CSF Leak Prevention: DuraSeal is highly effective in preventing CSF leaks, a major concern in spinal surgery.
- Biocompatible Material: The PEG-based composition is well-tolerated by the body, minimizing the risk of adverse reactions.
- Rapid Polymerization: The quick setting time allows for efficient sealing during surgery.
- Flexible and Elastic Seal: The sealant remains flexible and elastic, accommodating tissue movement without compromising the seal.
- Resorbable: DuraSeal is gradually resorbed by the body, eliminating the need for removal.
Cons/Limitations
- Requires a Dry Surgical Field: Moisture can interfere with adhesion, so a dry surgical field is essential.
- Not Suitable for Large Dural Defects: In cases of large dural defects, DuraSeal may not provide sufficient coverage.
- Cost: DuraSeal can be more expensive than traditional dural closure methods.
- Potential for Allergic Reactions: Although rare, allergic reactions to PEG-based sealants have been reported.
Ideal User Profile
DuraSeal is best suited for surgeons performing spinal procedures where there is a risk of CSF leakage, particularly in cases involving small to moderate dural defects. It is a valuable tool for both open and minimally invasive spinal surgeries. The sealant is particularly useful in patients with risk factors for CSF leakage, such as those with a history of prior spinal surgery or those undergoing complex reconstructions.
Key Alternatives
Alternatives to DuraSeal include other meningeal sealants, such as fibrin sealants and collagen matrices. Fibrin sealants are derived from human blood products and promote clot formation to seal dural defects. Collagen matrices provide a scaffold for tissue ingrowth and healing. While these alternatives can be effective, they may not offer the same level of strength and durability as DuraSeal.
Expert Overall Verdict & Recommendation
DuraSeal is a reliable and effective meningeal sealant that can significantly reduce the risk of CSF leakage in spinal surgery. Its biocompatibility, rapid polymerization, and strong adhesion make it a valuable tool for surgeons. While it has some limitations, such as the need for a dry surgical field and its unsuitability for large dural defects, its benefits generally outweigh its drawbacks. We recommend DuraSeal as a valuable adjunct to standard dural closure techniques in spinal surgery.
Understanding and Protecting Your Spinal Cord
In summary, the spinal cord membranes play a critical role in protecting and supporting the delicate neural tissue of the spinal cord. Understanding their anatomy, function, and clinical significance is essential for healthcare professionals and anyone interested in maintaining spinal health. By staying informed about the latest advancements in spinal cord membrane research and treatment, we can work towards improving the lives of individuals affected by disorders of these vital structures. We encourage you to discuss any concerns about your spinal health with your healthcare provider and to explore the resources available to learn more about this important topic. Share your experiences with spinal health maintenance and knowledge in the comments below.
</n
