Antithrombin 3 Deficiency: A Comprehensive Guide to Causes, Symptoms, and Management
Antithrombin 3 Deficiency, also known as Antithrombin Deficiency, is a rare genetic or acquired condition that significantly increases the risk of developing blood clots. This comprehensive guide delves into the intricacies of this often-overlooked disorder, providing you with the knowledge to understand its causes, recognize its symptoms, and explore the available management strategies. We aim to provide a more in-depth and practical understanding of this condition than is typically found in online resources, drawing on expert consensus and real-world observations.
What is Antithrombin 3 and Why Does Deficiency Matter?
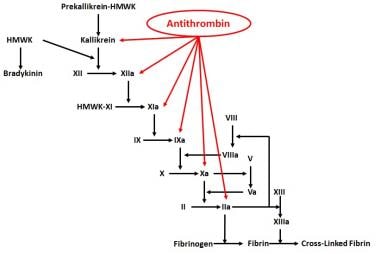
Antithrombin, also known as Antithrombin III (ATIII), is a naturally occurring protein in the blood that acts as a powerful anticoagulant. Its primary function is to inhibit several key enzymes in the coagulation cascade, effectively preventing excessive blood clot formation. Think of it as the body’s natural ‘blood thinner’. Without sufficient or properly functioning antithrombin, the delicate balance between clotting and bleeding shifts, predisposing individuals to a hypercoagulable state, or thrombophilia.
The importance of antithrombin lies in its role as a critical regulator of the coagulation system. When antithrombin levels are deficient, the body’s ability to control clot formation is compromised. This can lead to the development of dangerous blood clots in veins (venous thromboembolism or VTE) and arteries (arterial thrombosis), potentially causing life-threatening complications such as deep vein thrombosis (DVT), pulmonary embolism (PE), stroke, and even organ damage.
Types of Antithrombin 3 Deficiency: Inherited vs. Acquired
Antithrombin 3 Deficiency can be broadly classified into two main categories: inherited (genetic) and acquired.
- Inherited Antithrombin 3 Deficiency: This form is caused by genetic mutations in the SERPINC1 gene, which provides instructions for making antithrombin. These mutations can lead to either reduced levels of antithrombin (Type I) or the production of a dysfunctional antithrombin protein (Type II). Inherited deficiencies are typically present from birth and often have a more severe clinical presentation.
- Acquired Antithrombin 3 Deficiency: This form develops later in life due to various medical conditions or circumstances that reduce antithrombin levels. Common causes of acquired deficiency include:
- Liver disease (as the liver is responsible for producing antithrombin)
- Nephrotic syndrome (a kidney disorder that leads to protein loss in the urine, including antithrombin)
- Disseminated intravascular coagulation (DIC), a life-threatening condition that causes widespread blood clotting and consumption of clotting factors, including antithrombin
- Use of certain medications, such as heparin (in rare cases, can lead to heparin-induced thrombocytopenia and thrombosis – HIT/HITT)
- Severe trauma or surgery
- Pregnancy
Genetic Mutations and Their Impact on Antithrombin Function
The SERPINC1 gene is responsible for producing antithrombin. Mutations in this gene can result in various types of inherited antithrombin deficiency. These mutations can affect the quantity or quality of antithrombin produced.
- Type I Deficiency (Quantitative): In this type, the SERPINC1 gene mutation leads to reduced production of antithrombin, resulting in lower-than-normal levels of the protein in the blood.
- Type II Deficiency (Qualitative): In this type, the SERPINC1 gene mutation results in the production of a dysfunctional antithrombin protein. While the levels of antithrombin may be normal, the protein is unable to effectively inhibit coagulation enzymes. Type II deficiencies are further subdivided based on the specific functional defect:
- Type IIa: Affects the heparin-binding site of antithrombin, reducing its ability to be activated by heparin.
- Type IIb: Affects the reactive site of antithrombin, impairing its ability to bind to and inhibit target coagulation enzymes.
- Type IIc: Affects the antithrombin molecule in other ways, leading to impaired function.
Recognizing the Signs and Symptoms: What to Watch For
Many individuals with Antithrombin 3 Deficiency are asymptomatic until they experience a thrombotic event. Therefore, recognizing potential signs and symptoms is crucial for early diagnosis and management. Common signs and symptoms associated with blood clots include:
- Deep Vein Thrombosis (DVT): Pain, swelling, redness, and warmth in the affected leg (usually the calf or thigh).
- Pulmonary Embolism (PE): Sudden shortness of breath, chest pain (often sharp and stabbing), rapid heart rate, coughing up blood, and dizziness.
- Stroke: Sudden numbness or weakness of the face, arm, or leg (usually on one side of the body), difficulty speaking or understanding speech, vision problems, sudden severe headache, and loss of balance.
- Other Thrombotic Events: Depending on the location of the blood clot, other symptoms may include abdominal pain, limb ischemia (reduced blood flow to a limb), and organ damage.
It’s important to note that these symptoms are not specific to Antithrombin 3 Deficiency and can be caused by other conditions. However, if you experience any of these symptoms, especially if you have a family history of blood clots or other risk factors for thrombophilia, it’s crucial to seek medical attention promptly.
Diagnosis: Testing and Evaluation for Antithrombin 3 Deficiency
Diagnosing Antithrombin 3 Deficiency typically involves a combination of:
- Medical History and Physical Examination: Your doctor will ask about your personal and family history of blood clots, as well as any other relevant medical conditions or medications. A physical examination may help identify signs of DVT or other thrombotic events.
- Antithrombin Activity and Antigen Level Tests: These blood tests measure the level and function of antithrombin in your blood. Antithrombin activity tests assess how well antithrombin inhibits coagulation enzymes, while antithrombin antigen level tests measure the amount of antithrombin protein present.
- Genetic Testing: If inherited Antithrombin 3 Deficiency is suspected, genetic testing of the SERPINC1 gene can identify specific mutations.
- Other Thrombophilia Testing: Your doctor may also order other blood tests to evaluate for other inherited or acquired thrombophilias, such as Factor V Leiden mutation, Prothrombin G20210A mutation, Protein C deficiency, and Protein S deficiency.
It’s important to note that antithrombin levels can be affected by acute thrombosis, anticoagulant medications (such as heparin or warfarin), and certain medical conditions. Therefore, testing may need to be repeated at a later date to confirm the diagnosis.
Heparin’s Role in Antithrombin Activation
Heparin, a widely used anticoagulant medication, exerts its effects primarily by enhancing the activity of antithrombin. Heparin binds to antithrombin, causing a conformational change that dramatically increases its ability to inhibit coagulation enzymes, particularly thrombin and factor Xa. This interaction is crucial for heparin’s anticoagulant effect.
In individuals with Antithrombin 3 Deficiency, the effectiveness of heparin may be reduced, especially in those with Type I deficiency (reduced antithrombin levels). This is because there is less antithrombin available for heparin to activate. In these cases, higher doses of heparin may be required to achieve the desired anticoagulant effect, or alternative anticoagulants may be considered.
Management Strategies: Preventing and Treating Thrombotic Events
The management of Antithrombin 3 Deficiency focuses on preventing and treating thrombotic events. Strategies include:
- Anticoagulant Medications: These medications help prevent blood clots from forming or growing. Common anticoagulants used in the management of Antithrombin 3 Deficiency include:
- Heparin: An injectable anticoagulant that works by enhancing antithrombin activity. It’s often used for short-term anticoagulation, such as during pregnancy or before surgery.
- Warfarin (Coumadin): An oral anticoagulant that works by inhibiting the production of vitamin K-dependent clotting factors. It requires regular blood monitoring to ensure the correct dosage.
- Direct Oral Anticoagulants (DOACs): These newer oral anticoagulants, such as rivaroxaban (Xarelto), apixaban (Eliquis), edoxaban (Savaysa), and dabigatran (Pradaxa), directly inhibit specific coagulation enzymes. They offer the advantage of not requiring routine blood monitoring.
- Antithrombin Concentrate: In certain situations, such as during surgery or pregnancy, antithrombin concentrate (a purified form of antithrombin) may be administered to temporarily increase antithrombin levels.
- Thromboprophylaxis: Preventive measures to reduce the risk of blood clots. These may include:
- Compression stockings: To improve blood flow in the legs.
- Lifestyle modifications: Such as maintaining a healthy weight, staying active, and avoiding prolonged periods of sitting or standing.
- Prophylactic anticoagulation: Low-dose anticoagulants may be prescribed in high-risk situations, such as before surgery or during pregnancy.
Special Considerations: Pregnancy and Antithrombin 3 Deficiency
Pregnancy significantly increases the risk of blood clots, particularly in women with Antithrombin 3 Deficiency. Therefore, careful management is crucial during pregnancy and the postpartum period.
Management strategies may include:
- Prophylactic anticoagulation: Low-dose heparin or low molecular weight heparin (LMWH) is often prescribed throughout pregnancy and for several weeks postpartum to prevent blood clots.
- Monitoring antithrombin levels: Regular monitoring of antithrombin levels may be necessary to adjust the anticoagulant dosage.
- Delivery planning: The delivery plan should be carefully considered, with a focus on minimizing the risk of bleeding and thrombosis.
The Future of Antithrombin Deficiency Treatment: Emerging Therapies
While current management strategies are effective in preventing and treating thrombotic events in individuals with Antithrombin 3 Deficiency, research is ongoing to develop novel therapies. Some promising areas of research include:
- Gene therapy: To correct the underlying genetic defect in inherited Antithrombin 3 Deficiency.
- Novel anticoagulants: With improved safety and efficacy profiles.
- Personalized medicine: Tailoring treatment strategies based on an individual’s specific genetic makeup and clinical presentation.
Living with Antithrombin 3 Deficiency: Lifestyle Adjustments and Support
Living with Antithrombin 3 Deficiency requires ongoing management and lifestyle adjustments to minimize the risk of blood clots. Key recommendations include:
- Adhering to prescribed medications: Taking anticoagulant medications as prescribed and attending regular follow-up appointments.
- Maintaining a healthy lifestyle: Maintaining a healthy weight, staying active, and avoiding smoking.
- Avoiding prolonged periods of sitting or standing: Taking breaks to stretch and move around.
- Staying hydrated: Drinking plenty of fluids to prevent dehydration, which can increase the risk of blood clots.
- Wearing compression stockings: To improve blood flow in the legs, especially during travel or prolonged periods of sitting or standing.
- Informing healthcare providers: About your Antithrombin 3 Deficiency before any medical procedures or surgeries.
- Seeking support: Connecting with other individuals with Antithrombin 3 Deficiency and their families through support groups or online forums.
Seeking Expert Guidance: When to Consult a Specialist
If you suspect you may have Antithrombin 3 Deficiency, or if you have been diagnosed with the condition, it’s crucial to consult with a hematologist (a doctor specializing in blood disorders) or a thrombophilia specialist. These experts can provide comprehensive evaluation, diagnosis, and management strategies tailored to your individual needs. They can also help you navigate the complexities of living with Antithrombin 3 Deficiency and connect you with resources and support.
Understanding the Importance of Proactive Management
Antithrombin 3 Deficiency, while rare, poses a significant risk of life-threatening blood clots. By understanding the condition, recognizing its symptoms, and adhering to recommended management strategies, individuals with Antithrombin 3 Deficiency can significantly reduce their risk of thrombotic events and live full, active lives. Proactive management, in consultation with a hematologist or thrombophilia specialist, is key to ensuring optimal outcomes. If you believe you are at risk, consult your physician for an evaluation. Early diagnosis and treatment can make a significant difference.
