Navigating the Aetna Better Health Authorization Form in Louisiana: A Comprehensive Guide
Are you facing the often-confusing process of obtaining prior authorization from Aetna Better Health of Louisiana? You’re not alone. Navigating healthcare bureaucracy can be daunting, especially when it involves securing necessary approvals for medical services. This comprehensive guide is designed to demystify the Aetna Better Health authorization form for Louisiana, providing you with the knowledge and resources you need to successfully navigate the process. We aim to empower you with a clear understanding of the form, its requirements, and the steps involved in getting your healthcare needs approved. This guide reflects expert insights and practical advice to ensure you can confidently manage your healthcare journey with Aetna Better Health.
Understanding Prior Authorization with Aetna Better Health of Louisiana
Prior authorization, sometimes called pre-authorization or precertification, is a process used by health insurance companies like Aetna Better Health of Louisiana to determine if a particular medical service, treatment, prescription drug, or piece of durable medical equipment is medically necessary. In essence, it’s a way for Aetna to ensure that the care you receive is appropriate and cost-effective. The aetna better health authorization form for louisiana is the key document used to initiate this process.
The requirement for prior authorization isn’t arbitrary. It stems from a desire to manage healthcare costs, prevent unnecessary procedures, and ensure that members receive the most appropriate care based on evidence-based guidelines. Understanding this underlying rationale can help you approach the process with a more informed perspective.
Prior authorization requirements vary depending on your specific Aetna Better Health plan and the type of service you’re seeking. Some common services that often require prior authorization include:
- Inpatient hospital stays
- Certain outpatient procedures
- High-cost prescription medications
- Durable medical equipment (DME)
- Specialty care referrals (in some cases)
It’s crucial to consult your Aetna Better Health member handbook or contact their customer service to determine whether a specific service requires prior authorization. Failure to obtain prior authorization when required can result in denial of coverage, leaving you responsible for the full cost of the service.
Deciphering the Aetna Better Health Authorization Form for Louisiana
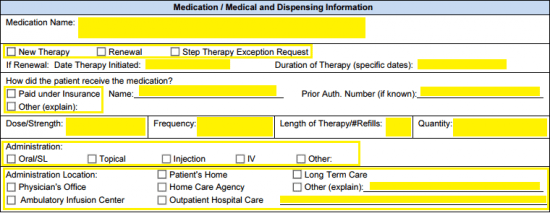
The aetna better health authorization form for louisiana is a standardized document that providers use to request prior authorization from Aetna Better Health. While the specific format may vary slightly over time, the core information requested remains consistent. Typically, the form will require the following details:
- Member Information: This includes the patient’s name, date of birth, Aetna Better Health member ID number, and contact information.
- Provider Information: This section requires the name, address, phone number, and National Provider Identifier (NPI) of the physician or healthcare provider requesting the authorization.
- Service Information: This is a detailed description of the specific service, treatment, medication, or equipment for which authorization is being requested. It should include the CPT (Current Procedural Terminology) or HCPCS (Healthcare Common Procedure Coding System) codes, as well as the diagnosis code (ICD-10).
- Clinical Information: This is perhaps the most critical section of the form. It requires the provider to provide detailed clinical documentation supporting the medical necessity of the requested service. This may include medical records, lab results, imaging reports, and a comprehensive explanation of the patient’s condition and why the requested service is appropriate.
- Supporting Documentation: Any additional documentation that supports the request, such as prior treatment records, specialist consultations, or relevant medical literature, should be included.
Completing the form accurately and thoroughly is essential for a successful prior authorization request. Missing or incomplete information can lead to delays or denials.
Step-by-Step Guide to Completing the Authorization Form
While the healthcare provider typically initiates and completes the aetna better health authorization form for louisiana, understanding the process can empower you to advocate for your healthcare needs. Here’s a step-by-step guide to the process:
- Confirm Prior Authorization Requirement: Before scheduling a service or filling a prescription, confirm with your provider and Aetna Better Health whether prior authorization is required.
- Gather Necessary Information: Ensure your provider has all the necessary information, including your Aetna Better Health member ID, relevant medical history, and any supporting documentation.
- Provider Completes the Form: The provider will complete the
aetna better health authorization form for louisiana, providing detailed information about the requested service and its medical necessity. - Submission to Aetna Better Health: The provider will submit the completed form and supporting documentation to Aetna Better Health through their preferred method (e.g., online portal, fax, or mail).
- Aetna Better Health Review: Aetna Better Health will review the request, often using clinical guidelines and medical necessity criteria to determine whether to approve or deny the authorization.
- Notification of Decision: Aetna Better Health will notify both the provider and the member of their decision. This notification will typically include the reason for the decision and any appeal rights.
It’s important to note that the timeframe for Aetna Better Health to review and process prior authorization requests can vary. Urgent requests are typically expedited, while routine requests may take several business days.
Strategies for a Successful Prior Authorization Request
Increasing your chances of a successful prior authorization request involves proactive communication and attention to detail. Consider these strategies:
- Proactive Communication: Discuss the need for prior authorization with your provider well in advance of the scheduled service. This allows ample time to gather necessary information and complete the form.
- Thorough Documentation: Ensure your provider includes comprehensive and detailed clinical documentation supporting the medical necessity of the requested service. This should include relevant medical history, physical examination findings, lab results, imaging reports, and a clear explanation of why the service is appropriate for your condition.
- Adherence to Guidelines: Familiarize yourself with Aetna Better Health’s clinical guidelines for the specific service you’re seeking. These guidelines outline the criteria that Aetna uses to determine medical necessity. Your provider should be aware of these guidelines and ensure that the request aligns with them.
- Peer-to-Peer Review: If your request is initially denied, your provider can request a peer-to-peer review with a medical director at Aetna Better Health. This allows for a direct discussion of the case and an opportunity to address any concerns or questions.
- Member Advocacy: As a member, you have the right to advocate for your healthcare needs. Contact Aetna Better Health’s member services to inquire about the status of your request, understand the reasons for a denial, and explore your appeal options.
Aetna Better Health’s Online Resources: A Digital Approach
Aetna Better Health provides a variety of online resources that can assist you with the prior authorization process. These resources may include:
- Provider Portal: A secure online portal where providers can submit prior authorization requests, check the status of existing requests, and access clinical guidelines.
- Form Repository: A library of downloadable forms, including the
aetna better health authorization form for louisiana, and other relevant documents. - Frequently Asked Questions (FAQs): A comprehensive list of FAQs addressing common questions about prior authorization, coverage, and other member-related topics.
- Member Handbook: A detailed handbook outlining your Aetna Better Health plan benefits, coverage rules, and prior authorization requirements.
Navigating these online resources can streamline the prior authorization process and provide you with valuable information.
Understanding Aetna’s Coverage Determination Process
Aetna Better Health utilizes a structured coverage determination process to evaluate prior authorization requests. This process typically involves the following steps:
- Initial Review: A team of nurses or medical professionals reviews the request to ensure that all necessary information is included and that the requested service is covered under the member’s plan.
- Medical Necessity Review: If the request meets the initial criteria, it is then reviewed by a medical director or physician advisor who specializes in the relevant area of medicine. This reviewer assesses the medical necessity of the requested service based on clinical guidelines, evidence-based literature, and the patient’s specific medical condition.
- Decision and Notification: Based on the medical necessity review, Aetna Better Health will either approve or deny the request. The provider and member will be notified of the decision, along with the rationale behind it.
Understanding this process can help you anticipate the types of information and documentation that Aetna Better Health will be looking for when evaluating your prior authorization request.
Navigating Denials and Appealing Decisions
If your prior authorization request is denied, it’s important to understand your appeal rights. Aetna Better Health provides a formal appeal process that allows you to challenge the denial and request a reconsideration of the decision.
The appeal process typically involves the following steps:
- Filing an Appeal: You must file a written appeal within a specified timeframe (typically 60 days from the date of the denial notice). The appeal should clearly state the reasons why you believe the denial was incorrect and include any additional information or documentation that supports your case.
- Internal Review: Aetna Better Health will conduct an internal review of the appeal, often by a different medical director or physician advisor than the one who made the initial decision.
- External Review: If the internal review upholds the denial, you may have the right to request an external review by an independent review organization (IRO). The IRO is a third-party organization that is not affiliated with Aetna Better Health and is responsible for making an impartial decision on the appeal.
Throughout the appeal process, it’s crucial to maintain open communication with Aetna Better Health and your healthcare provider. Seek guidance from patient advocacy organizations or legal counsel if needed.
The Role of Technology in Streamlining Authorizations
Aetna Better Health, like many modern insurers, is increasingly leveraging technology to streamline the prior authorization process. Electronic prior authorization (ePA) systems allow providers to submit requests electronically, receive real-time status updates, and communicate securely with Aetna Better Health. These systems offer several advantages:
- Faster Processing Times: ePA systems can significantly reduce the time it takes to process prior authorization requests.
- Improved Accuracy: Electronic submission reduces the risk of errors associated with manual paperwork.
- Enhanced Transparency: Providers and members can track the status of requests in real-time.
Ask your provider if they utilize ePA systems when submitting prior authorization requests to Aetna Better Health.
Aetna Better Health’s Commitment to Member Support
Aetna Better Health is committed to providing its members with the support and resources they need to navigate the healthcare system. This commitment is reflected in their member services programs, which include:
- Dedicated Member Services Representatives: A team of trained representatives who can answer your questions, provide guidance on coverage and benefits, and assist with prior authorization inquiries.
- Care Management Programs: Programs designed to help members manage chronic health conditions and improve their overall health outcomes.
- Health Education Resources: A variety of educational materials, including brochures, videos, and online resources, that provide information on health topics and preventive care.
Don’t hesitate to reach out to Aetna Better Health’s member services for assistance with any questions or concerns you may have about the prior authorization process or your healthcare coverage.
Empowering Your Healthcare Journey with Aetna Better Health
Understanding the intricacies of the aetna better health authorization form for louisiana and the broader prior authorization process is crucial for navigating your healthcare journey with confidence. By proactively communicating with your provider, gathering necessary information, and familiarizing yourself with Aetna Better Health’s policies and procedures, you can increase your chances of a successful outcome. Remember, you have the right to advocate for your healthcare needs and to appeal decisions that you believe are incorrect. Aetna Better Health is dedicated to supporting its members and providing the resources they need to access quality healthcare.
