Famotidine for Infants: A Comprehensive Guide for Parents
Is your infant experiencing discomfort from acid reflux? As a parent, seeing your little one in distress is heartbreaking. If your pediatrician has suggested famotidine for infants, you’re likely searching for reliable information about its use, benefits, and potential side effects. This comprehensive guide aims to provide you with the knowledge and understanding you need to make informed decisions about your child’s health. We will delve into the specifics of famotidine, its mechanism of action, appropriate dosages, potential side effects, and crucial precautions. Our goal is to empower you with a comprehensive understanding, ensuring you feel confident in navigating your infant’s health journey. This is not a substitute for professional medical advice, diagnosis, or treatment, and it is essential to consult with your pediatrician or other qualified healthcare provider for any questions you may have regarding a medical condition or treatment.
Understanding Infant Acid Reflux and the Role of Famotidine
Gastroesophageal reflux (GER), commonly known as acid reflux, is a frequent occurrence in infants. It happens when stomach contents flow back up into the esophagus. This can be due to the immaturity of the lower esophageal sphincter (LES), the muscle that prevents stomach acid from flowing back up. While some reflux is normal and often resolves on its own as the infant matures, excessive or problematic reflux, known as gastroesophageal reflux disease (GERD), can cause significant discomfort and complications.
Symptoms of GERD in infants can include:
- Frequent spitting up or vomiting
- Irritability and crying, especially after feeding
- Poor weight gain or weight loss
- Refusal to feed
- Arching the back during or after feeding
- Coughing or wheezing
- Sleep disturbances
Famotidine, a histamine-2 receptor antagonist (H2RA), works by reducing the amount of acid produced in the stomach. By decreasing stomach acid, famotidine can help alleviate the symptoms of GERD in infants, allowing the esophagus to heal and reducing discomfort. It is crucial to understand that famotidine does not stop reflux from occurring; it simply makes the refluxed material less acidic and, therefore, less irritating.
Famotidine: A Closer Look at its Mechanism and Formulation
Famotidine belongs to a class of drugs called H2 receptor antagonists. These drugs work by blocking the action of histamine on the histamine H2 receptors in the stomach. Histamine stimulates the parietal cells in the stomach to produce acid. By blocking histamine, famotidine reduces acid production. This makes the stomach contents less acidic, reducing irritation to the esophagus when reflux occurs.
Famotidine is available in several formulations, including:
- Oral Suspension: A liquid form that is commonly prescribed for infants due to ease of administration and accurate dosing.
- Tablets: Available in various strengths, but typically not used for infants unless compounded into a liquid form by a pharmacist.
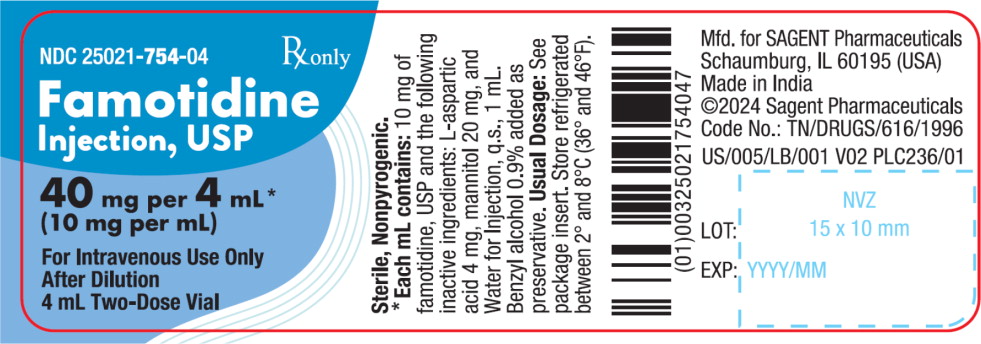
- Injection: Used in hospital settings for infants who cannot take oral medication.
For infants, the oral suspension is the preferred formulation due to its ease of use and ability to provide accurate dosing based on the infant’s weight. Compounding pharmacies can also create custom formulations and dosages if needed, based on a prescription from the infant’s doctor.
Dosage Guidelines for Famotidine in Infants: A Precise Approach
Important Note: The dosage of famotidine for infants is highly individualized and should only be determined by a qualified pediatrician or healthcare provider. This section provides general information but is not a substitute for professional medical advice.
The typical dosage of famotidine for infants is based on their weight and is usually administered once or twice daily. A healthcare professional will calculate the precise dosage based on the infant’s specific needs and medical condition. It’s imperative to follow the prescribed dosage meticulously.
Factors influencing the dosage include:
- Infant’s Weight: Dosage is calculated in milligrams per kilogram (mg/kg).
- Severity of Reflux: More severe cases may require higher doses.
- Kidney Function: Infants with impaired kidney function may require a lower dose.
- Other Medications: Certain medications can interact with famotidine, requiring dosage adjustments.
Accurate measurement of the dosage is crucial. Use a calibrated oral syringe or measuring device to ensure you are giving the correct amount. Never use household teaspoons or tablespoons, as they are not accurate.
Administering Famotidine to Infants: Practical Tips and Techniques
Giving medication to an infant can sometimes be challenging. Here are some practical tips to help you administer famotidine effectively:
- Use an Oral Syringe: An oral syringe allows for accurate dosing and easy administration. Draw up the prescribed amount of famotidine into the syringe.
- Positioning: Hold your infant in a semi-upright position. This helps prevent choking and ensures the medication goes down smoothly.
- Administer Slowly: Gently squirt the medication into the side of your infant’s mouth, towards the cheek. This allows them to swallow the medication gradually and reduces the risk of spitting up.
- Mix with a Small Amount of Food (If Approved): If your infant is resistant to taking the medication, you can try mixing it with a very small amount of breast milk or formula. However, always check with your pediatrician or pharmacist first to ensure this is appropriate and won’t affect the medication’s effectiveness.
- Consistency is Key: Administer the medication at the same time(s) each day to maintain a consistent level in your infant’s system.
Potential Side Effects of Famotidine in Infants: What to Watch For
While famotidine is generally considered safe for infants, it’s essential to be aware of potential side effects. Most side effects are mild and resolve on their own. However, if you notice any concerning symptoms, contact your pediatrician immediately.
Common side effects may include:
- Irritability: Some infants may become more irritable or fussy while taking famotidine.
- Diarrhea or Constipation: Changes in bowel habits can occur.
- Dry Mouth: Famotidine can sometimes cause dry mouth.
- Headache: Although rare in infants, headache is a potential side effect.
Rare but serious side effects include:
- Allergic Reactions: Symptoms may include rash, hives, itching, swelling, difficulty breathing, or anaphylaxis. Seek immediate medical attention if you suspect an allergic reaction.
- Seizures: Although extremely rare, seizures have been reported in some cases.
- Irregular Heartbeat: Another very rare but serious side effect.
Long-term use of famotidine may also have potential effects, such as an increased risk of certain infections or nutrient deficiencies. Discuss the potential risks and benefits of long-term famotidine use with your pediatrician.
Precautions and Contraindications: Ensuring Safe Use of Famotidine
Before starting famotidine, inform your pediatrician about your infant’s complete medical history, including any allergies, existing medical conditions, and current medications. Certain conditions may warrant caution or contraindicate the use of famotidine.
Precautions to consider:
- Kidney Disease: Infants with kidney disease may require a lower dose of famotidine.
- Liver Disease: Use famotidine with caution in infants with liver disease.
- Allergies: Do not use famotidine in infants who are allergic to it or other H2 receptor antagonists.
- Phenylketonuria (PKU): Some liquid formulations of famotidine may contain phenylalanine, which can be harmful to infants with PKU. Check the product label carefully.
Famotidine can interact with certain medications, including:
- Antacids: Antacids can decrease the absorption of famotidine. Administer antacids at least 1-2 hours apart from famotidine.
- Ketoconazole and Itraconazole: Famotidine can reduce the absorption of these antifungal medications.
- Calcium Carbonate: Famotidine can decrease the absorption of calcium carbonate.
Always consult with your pediatrician or pharmacist before giving your infant any new medication, including over-the-counter drugs, herbal remedies, or supplements.
Lifestyle Modifications and Alternative Therapies for Infant Reflux
In addition to famotidine, several lifestyle modifications and alternative therapies can help manage infant reflux:
- Feeding Techniques: Feed your infant in an upright position and keep them upright for at least 30 minutes after feeding.
- Smaller, More Frequent Feedings: Smaller feedings can reduce the pressure on the lower esophageal sphincter.
- Burping Frequently: Burp your infant frequently during and after feedings to release trapped air.
- Thickening Feeds: In some cases, thickening breast milk or formula with rice cereal may help reduce reflux. However, always consult with your pediatrician before thickening feeds, as it can have potential risks.
- Probiotics: Some studies suggest that probiotics may help reduce reflux symptoms in infants.
- Chiropractic Care: Some parents seek chiropractic care for infants with reflux, although the evidence supporting its effectiveness is limited.
It’s important to discuss any alternative therapies with your pediatrician before trying them, as some may not be safe or effective for infants.
When to Seek Immediate Medical Attention for Infant Reflux
While most cases of infant reflux are mild and resolve on their own or with treatment, certain symptoms warrant immediate medical attention:
- Forceful Vomiting: Projectile vomiting can be a sign of pyloric stenosis, a condition that requires surgical intervention.
- Blood in Vomit or Stool: This can indicate damage to the esophagus or other parts of the digestive tract.
- Difficulty Breathing: Reflux can sometimes cause aspiration, leading to breathing difficulties.
- Severe Irritability or Lethargy: These symptoms can indicate a serious underlying condition.
- Dehydration: Signs of dehydration include decreased urination, dry mouth, and sunken eyes.
- Failure to Thrive: Poor weight gain or weight loss can be a sign of a more serious problem.
If your infant experiences any of these symptoms, seek immediate medical attention.
Famotidine vs. Other Reflux Medications: A Comparative Overview
Famotidine is not the only medication used to treat infant reflux. Other options include:
- Ranitidine (Zantac): Another H2 receptor antagonist that works similarly to famotidine. However, ranitidine has been recalled from the market due to concerns about contamination with a potential carcinogen.
- Proton Pump Inhibitors (PPIs): PPIs, such as omeprazole and lansoprazole, are more potent acid-reducing medications than H2 receptor antagonists. They work by blocking the enzyme that produces stomach acid. PPIs are generally reserved for more severe cases of GERD in infants due to potential long-term side effects.
- Antacids: Antacids neutralize stomach acid but do not reduce acid production. They provide temporary relief but are not a long-term solution.
Each medication has its own set of benefits and risks. Your pediatrician will determine the best option for your infant based on their individual needs and medical history.
The Importance of Ongoing Communication with Your Pediatrician
Managing infant reflux often requires a collaborative approach between parents and healthcare providers. Regular communication with your pediatrician is crucial to ensure your infant is receiving the best possible care.
Be sure to:
- Report any changes in your infant’s symptoms or condition.
- Ask questions about any concerns you have.
- Follow your pediatrician’s instructions carefully.
- Attend all scheduled follow-up appointments.
By working closely with your pediatrician, you can help your infant find relief from reflux symptoms and thrive.
Finding Comfort and Relief for Your Little One
Dealing with infant reflux can be a challenging and stressful experience for parents. Understanding the role of famotidine for infants, its proper use, potential side effects, and alternative management strategies is crucial for providing the best possible care for your little one. Remember that every infant is unique, and what works for one may not work for another. Close collaboration with your pediatrician, combined with patience and persistence, is key to finding the right approach to manage your infant’s reflux and ensure their comfort and well-being. If you are looking for further resources, do not hesitate to contact your doctor or other qualified healthcare provider.
