Understanding Colorectal Cancer: A Comprehensive Guide
Colorectal cancer, encompassing cancers of the colon and rectum, represents a significant health challenge worldwide. Early detection and advancements in treatment have dramatically improved outcomes, making knowledge and proactive screening crucial. This comprehensive guide aims to provide you with the information you need to understand colorectal cancer, its risk factors, prevention strategies, diagnostic methods, and the latest treatment options. We delve into the complexities of this disease, offering practical insights and expert perspectives to empower you and your loved ones.
What is Colorectal Cancer? A Deep Dive
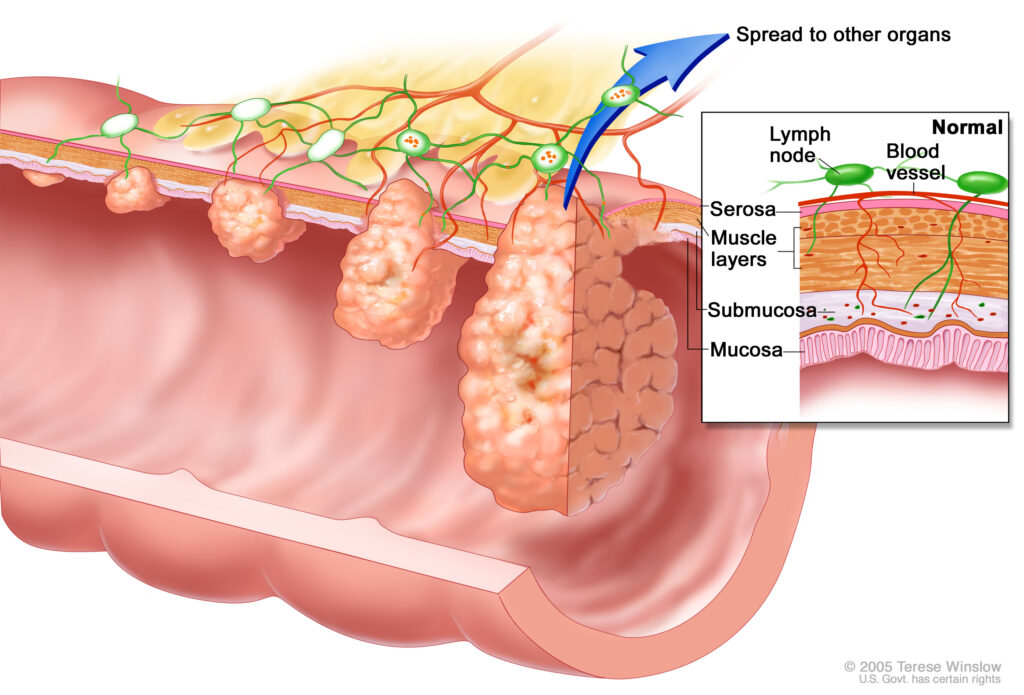
Colorectal cancer begins when abnormal cells develop in the lining of the colon or rectum. These cells can form growths called polyps. While most polyps are benign, some can become cancerous over time. The transformation from a benign polyp to a malignant tumor is a gradual process, often taking several years. Understanding this progression is vital for effective prevention through screening and early intervention.
The colon and rectum are parts of the large intestine, responsible for processing waste from digested food. The colon absorbs water and nutrients, while the rectum stores waste until it is eliminated. Cancers in these areas can disrupt these functions, leading to various symptoms and health complications. The location of the cancer (colon vs. rectum) can influence the treatment approach.
Colorectal cancer is not a single disease but rather a group of diseases with different molecular characteristics and behaviors. These differences can impact how the cancer responds to treatment. Researchers are continually working to identify these subtypes and develop more targeted therapies.
The Importance of Early Detection and Screening
Early detection is paramount in improving survival rates for colorectal cancer. Screening tests can detect polyps or cancer at an early stage, when treatment is most effective. Regular screening is recommended for individuals at average risk starting at age 45. However, those with a family history of colorectal cancer, certain genetic syndromes, or inflammatory bowel disease may need to begin screening earlier and undergo more frequent testing.
Screening options include colonoscopy, sigmoidoscopy, stool-based tests (such as fecal occult blood test (FOBT) and fecal immunochemical test (FIT)), and CT colonography (virtual colonoscopy). Colonoscopy remains the gold standard, allowing for both detection and removal of polyps during the same procedure. Stool-based tests are less invasive but require more frequent testing and may need to be followed up with a colonoscopy if abnormal results are found.
The choice of screening test should be made in consultation with your doctor, considering your individual risk factors, preferences, and access to resources. Adherence to recommended screening guidelines is crucial for reducing the incidence and mortality of colorectal cancer.
Understanding the Molecular Basis of Colorectal Cancer
Recent advances in molecular biology have revealed that colorectal cancer is not a single disease, but rather a collection of diseases driven by different genetic and epigenetic alterations. Key genes involved in colorectal cancer development include APC, KRAS, TP53, and microsatellite instability (MSI) genes. Mutations in these genes can disrupt normal cell growth and division, leading to the formation of cancerous tumors.
Understanding the molecular profile of a patient’s tumor can help guide treatment decisions. For example, tumors with MSI-high status are often more responsive to immunotherapy. Similarly, patients with KRAS mutations may not benefit from certain targeted therapies. Molecular testing is becoming increasingly important in personalizing treatment for colorectal cancer patients.
Risk Factors for Colorectal Cancer
Several factors can increase your risk of developing colorectal cancer. Some risk factors are modifiable, while others are not. Modifiable risk factors include:
- Diet: A diet high in red and processed meats and low in fiber is associated with an increased risk.
- Obesity: Being overweight or obese increases the risk of colorectal cancer in both men and women.
- Physical inactivity: A sedentary lifestyle contributes to an increased risk.
- Smoking: Smoking is linked to an increased risk of colorectal cancer, as well as other cancers.
- Alcohol consumption: Heavy alcohol consumption is associated with an increased risk.
Non-modifiable risk factors include:
- Age: The risk of colorectal cancer increases with age, with most cases occurring in people over 50.
- Family history: Having a family history of colorectal cancer or polyps increases your risk.
- Personal history: A personal history of colorectal cancer, polyps, or inflammatory bowel disease increases your risk.
- Genetic syndromes: Certain genetic syndromes, such as familial adenomatous polyposis (FAP) and Lynch syndrome, significantly increase the risk.
- Race and ethnicity: African Americans have the highest incidence and mortality rates of colorectal cancer in the United States.
Prevention Strategies for Colorectal Cancer
While not all risk factors can be avoided, adopting a healthy lifestyle can significantly reduce your risk of developing colorectal cancer. Key prevention strategies include:
- Maintain a healthy weight: Achieve and maintain a healthy weight through diet and exercise.
- Eat a healthy diet: Focus on a diet rich in fruits, vegetables, and whole grains, and limit red and processed meats.
- Get regular exercise: Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic exercise per week.
- Quit smoking: If you smoke, quitting is one of the best things you can do for your health.
- Limit alcohol consumption: If you drink alcohol, do so in moderation.
- Get screened regularly: Follow recommended screening guidelines for colorectal cancer.
Symptoms of Colorectal Cancer
In its early stages, colorectal cancer may not cause any symptoms. As the cancer grows, it can lead to various symptoms, including:
- Changes in bowel habits: Diarrhea, constipation, or narrowing of the stool that lasts for more than a few days.
- Rectal bleeding: Blood in the stool or rectal bleeding.
- Abdominal discomfort: Cramps, gas, or pain in the abdomen.
- Weakness or fatigue: Feeling tired or weak.
- Unexplained weight loss: Losing weight without trying.
It’s important to note that these symptoms can also be caused by other conditions. However, if you experience any of these symptoms, it’s crucial to see your doctor for evaluation.
Diagnosis of Colorectal Cancer
If your doctor suspects you may have colorectal cancer, they will perform a physical exam and order various tests, including:
- Colonoscopy: A colonoscopy is the most common diagnostic test for colorectal cancer. During a colonoscopy, a long, flexible tube with a camera attached is inserted into the rectum and advanced through the colon. This allows the doctor to visualize the entire colon and rectum and remove any polyps or suspicious tissue for biopsy.
- Sigmoidoscopy: A sigmoidoscopy is similar to a colonoscopy, but it only examines the lower portion of the colon (the sigmoid colon).
- Biopsy: A biopsy involves removing a sample of tissue for examination under a microscope. A biopsy is necessary to confirm a diagnosis of colorectal cancer.
- Imaging tests: Imaging tests, such as CT scans and MRI scans, can help determine the extent of the cancer and whether it has spread to other parts of the body.
Treatment Options for Colorectal Cancer
Treatment for colorectal cancer depends on several factors, including the stage of the cancer, its location, and your overall health. Common treatment options include:
- Surgery: Surgery is the primary treatment for most cases of colorectal cancer. The goal of surgery is to remove the cancer and any nearby lymph nodes that may contain cancer cells.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It may be used before or after surgery, or as the primary treatment for advanced cancer.
- Radiation therapy: Radiation therapy uses high-energy rays to kill cancer cells. It may be used before or after surgery, or as the primary treatment for rectal cancer.
- Targeted therapy: Targeted therapy uses drugs that target specific molecules involved in cancer cell growth and survival. It may be used for advanced cancer.
- Immunotherapy: Immunotherapy uses drugs that help your immune system fight cancer. It may be used for advanced cancer with certain genetic characteristics.
Treatment for colorectal cancer is often a multidisciplinary approach, involving surgeons, medical oncologists, radiation oncologists, and other specialists. The treatment plan will be tailored to your individual needs and circumstances.
Innovations in Colorectal Cancer Treatment: Immunotherapy’s Promise
Immunotherapy represents a significant advancement in cancer treatment, particularly for certain subsets of colorectal cancer patients. Unlike traditional chemotherapy, which directly targets cancer cells, immunotherapy harnesses the power of the patient’s own immune system to recognize and destroy cancer cells. One promising area is the use of checkpoint inhibitors, which block proteins that prevent the immune system from attacking cancer cells. Studies have shown that patients with microsatellite instability-high (MSI-H) colorectal cancer, characterized by a high number of genetic mutations, often respond well to immunotherapy. This personalized approach to treatment is transforming the landscape of colorectal cancer care, offering new hope for patients with advanced disease. Our experience shows that combining immunotherapy with other treatments can lead to better outcomes.
The Role of Diet and Lifestyle After Colorectal Cancer Treatment
Adopting a healthy diet and lifestyle after colorectal cancer treatment is crucial for recovery and reducing the risk of recurrence. Focus on a diet rich in fruits, vegetables, and whole grains, and limit red and processed meats. Regular exercise can also help improve your overall health and reduce the risk of recurrence. Based on expert consensus, maintaining a healthy weight is also vital. It’s also important to follow up with your doctor for regular checkups and screening tests.
Living with Colorectal Cancer: Support and Resources
Living with colorectal cancer can be challenging, both physically and emotionally. It’s important to have a strong support system in place. This may include family, friends, support groups, and healthcare professionals. Many resources are available to help you cope with the challenges of colorectal cancer, including:
- The American Cancer Society: Provides information, resources, and support for people with cancer and their families.
- The Colorectal Cancer Alliance: Offers support, advocacy, and education for people affected by colorectal cancer.
- The National Cancer Institute: Provides comprehensive information about cancer, including colorectal cancer.
A Brighter Future Through Awareness and Action
Colorectal cancer is a serious disease, but it is also preventable and treatable, especially when detected early. By understanding the risk factors, adopting healthy lifestyle habits, and getting screened regularly, you can significantly reduce your risk of developing colorectal cancer. Recent studies indicate that increased awareness and access to screening have led to a decline in colorectal cancer rates in recent years. If you or a loved one is facing a diagnosis of colorectal cancer, remember that you are not alone. Many resources are available to help you navigate the challenges of this disease. Contact our experts for a consultation on colorectal cancer. Your health is your most valuable asset; take proactive steps to protect it.
