Decoding ANA Positive ICD-10: A Comprehensive Guide
If you’ve encountered the term “ANA positive ICD-10,” you’re likely seeking clarity on what it signifies, its implications for your health, and how it’s classified within the medical coding system. This comprehensive guide aims to provide a detailed understanding of ANA (antinuclear antibody) positive results in the context of ICD-10 (International Classification of Diseases, Tenth Revision) coding. We’ll delve into the nuances of ANA testing, explore the conditions associated with positive results, and explain how these are represented within the ICD-10 framework. Our goal is to empower you with the knowledge to navigate this complex topic with confidence.
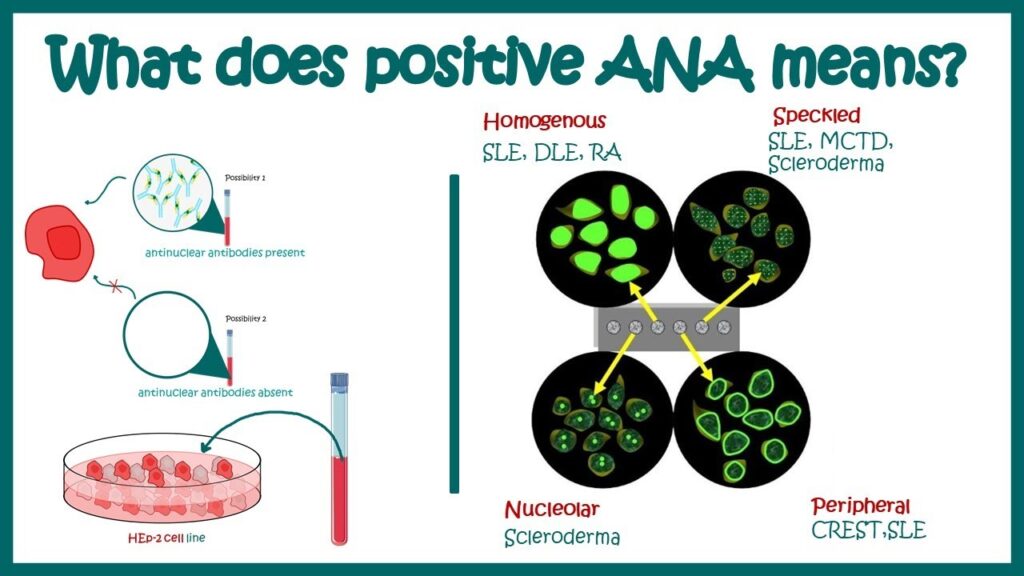
Understanding Antinuclear Antibodies (ANA)
Antinuclear antibodies (ANAs) are a group of autoantibodies that bind to components within the cell nucleus. These antibodies are produced by the immune system when it mistakenly attacks the body’s own tissues. An ANA test is a blood test that detects the presence of these antibodies. A positive ANA test indicates that ANAs are present in the blood, but it doesn’t necessarily mean that a person has an autoimmune disease. According to rheumatology experts, the presence of ANA should always be interpreted in conjunction with clinical findings and other laboratory tests.
The Significance of a Positive ANA Result
A positive ANA result can be associated with various autoimmune diseases, including:
- Systemic lupus erythematosus (SLE)
- Sjögren’s syndrome
- Systemic sclerosis (scleroderma)
- Polymyositis and dermatomyositis
- Mixed connective tissue disease (MCTD)
- Rheumatoid arthritis
However, it’s crucial to understand that a positive ANA result can also occur in healthy individuals, particularly in older adults. Furthermore, certain infections, medications, and other non-autoimmune conditions can also trigger a positive ANA. Therefore, a positive ANA result alone is not sufficient to diagnose an autoimmune disease.
ANA Titers and Patterns
When an ANA test is performed, the results are reported as a titer and a pattern. The titer represents the concentration of ANAs in the blood. A higher titer generally indicates a greater likelihood of an autoimmune disease, but this is not always the case. The pattern refers to the staining pattern observed under a microscope when the ANA test is performed. Different patterns can be associated with different autoimmune diseases. Common ANA patterns include:
- Homogeneous: Often seen in SLE and drug-induced lupus
- Speckled: Associated with various autoimmune diseases, including Sjögren’s syndrome, scleroderma, and MCTD
- Nucleolar: More specific for scleroderma
- Centromere: Also associated with scleroderma, particularly the limited cutaneous form (CREST syndrome)
ICD-10 Coding: The Basics
The International Classification of Diseases, Tenth Revision (ICD-10) is a standardized coding system used to classify and code diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases. It’s used worldwide for morbidity and mortality statistics, reimbursement, and clinical decision support. In the United States, a modified version called ICD-10-CM (Clinical Modification) is used for diagnosis coding.
The Purpose of ICD-10 Coding
ICD-10 codes provide a standardized way to communicate medical information. They allow healthcare providers, insurance companies, and public health agencies to track and analyze health trends, monitor disease outbreaks, and improve healthcare delivery. Accurate ICD-10 coding is essential for proper reimbursement for medical services.
ANA Positive ICD-10: How It Works
The term “ANA positive ICD-10” doesn’t refer to a specific ICD-10 code for a positive ANA test itself. Instead, it refers to the process of assigning the appropriate ICD-10 code(s) to the underlying condition or disease that is causing the positive ANA result. Because a positive ANA can be associated with a wide range of conditions, the correct ICD-10 code will vary depending on the specific diagnosis.
Finding the Right Code
The process of assigning an ICD-10 code for an ANA-positive patient involves several steps:
- Determine the underlying diagnosis: This is the most crucial step. The healthcare provider must determine the specific disease or condition that is causing the positive ANA result. This may involve further testing, such as specific autoantibody tests (e.g., anti-dsDNA, anti-Ro/SSA, anti-La/SSB), imaging studies, and clinical evaluation.
- Consult the ICD-10-CM coding manual or electronic coding resource: Once the diagnosis is established, the coder will use the ICD-10-CM coding manual or an electronic coding resource to find the appropriate code.
- Follow coding guidelines: The ICD-10-CM coding manual includes specific guidelines for coding various conditions. It’s essential to follow these guidelines to ensure accurate coding.
- Code to the highest level of specificity: ICD-10-CM codes can range from general to very specific. The coder should assign the code that is most specific to the patient’s condition.
Common ICD-10 Codes Associated with ANA Positive Results
Here are some examples of ICD-10 codes that may be associated with a positive ANA result, depending on the underlying diagnosis:
- M32.9: Systemic lupus erythematosus, unspecified: This code is used when a patient has SLE, but the specific type or manifestation is not specified.
- M35.0: Sicca syndrome [Sjögren’s]: This code is used for Sjögren’s syndrome, an autoimmune disease that affects the moisture-producing glands.
- M34.0: Systemic sclerosis: This code is used for systemic sclerosis (scleroderma), a chronic autoimmune disease that affects the skin and internal organs.
- M33.20: Polymyositis, unspecified: This code is used for polymyositis, an inflammatory muscle disease.
- M35.1: Other overlap syndromes: This code is used for mixed connective tissue disease (MCTD), an autoimmune disease that has features of SLE, scleroderma, and polymyositis.
- M05.9: Rheumatoid arthritis, unspecified: This code is used for rheumatoid arthritis, a chronic inflammatory disorder that affects the joints.
- R77.9: Abnormality of plasma protein, unspecified: This code might be used when a positive ANA is present, but the underlying cause has not yet been determined. It is generally not appropriate as a final diagnosis code.
Important Note: This is not an exhaustive list, and the appropriate ICD-10 code will depend on the specific clinical findings and diagnosis.
The Role of the Healthcare Provider
The healthcare provider plays a critical role in determining the underlying cause of a positive ANA result and assigning the correct ICD-10 code. The provider will consider the patient’s medical history, physical examination findings, and the results of other laboratory tests to arrive at a diagnosis. They will then use their clinical judgment to select the most appropriate ICD-10 code(s) to accurately reflect the patient’s condition.
Communication is Key
Effective communication between the healthcare provider and the medical coder is essential for accurate ICD-10 coding. The provider should clearly document the patient’s diagnosis and any relevant clinical information in the medical record. The coder should review the medical record carefully and ask the provider for clarification if needed.
Navigating the Complexity: Best Practices
Accurate ICD-10 coding for patients with positive ANA results can be challenging due to the wide range of potential underlying conditions. Here are some best practices to ensure accurate and efficient coding:
- Stay up-to-date with ICD-10-CM coding guidelines: The ICD-10-CM coding guidelines are updated annually. Coders should stay informed of any changes to the guidelines.
- Use reliable coding resources: There are many electronic coding resources available that can assist coders in finding the correct ICD-10 codes.
- Seek clarification when needed: If a coder is unsure about the correct ICD-10 code to assign, they should consult with the healthcare provider or a certified coding specialist.
- Document everything: Thorough documentation is essential for accurate coding and billing. The medical record should clearly reflect the patient’s diagnosis, clinical findings, and treatment plan.
ANA Testing: Understanding the Process
The ANA test is a common blood test used to help diagnose autoimmune disorders. Understanding the testing process can help patients better interpret their results and communicate with their healthcare providers.
Preparing for the Test
Generally, no special preparation is needed before an ANA test. Patients should inform their doctor about any medications they are taking, as some drugs can interfere with the results. The test involves a simple blood draw, usually from a vein in the arm.
Interpreting the Results
As mentioned earlier, ANA results are reported as a titer and a pattern. The titer indicates the amount of antibodies present, while the pattern describes the appearance of the antibodies under a microscope. A positive ANA result means that antibodies were detected, but further testing is usually required to determine the underlying cause. A negative ANA result makes an autoimmune disease less likely, but it doesn’t completely rule it out.
Beyond the Basics: Advanced Considerations
For healthcare professionals, understanding the nuances of ANA testing and ICD-10 coding is crucial for providing optimal patient care. Here are some advanced considerations:
The Importance of Specific Autoantibody Testing
If an ANA test is positive, specific autoantibody tests can help narrow down the diagnosis. These tests detect antibodies that are specific to certain autoimmune diseases. For example, anti-dsDNA antibodies are highly specific for SLE, while anti-Ro/SSA and anti-La/SSB antibodies are commonly found in Sjögren’s syndrome.
The Role of Clinical Correlation
It’s essential to correlate ANA results with the patient’s clinical presentation. A positive ANA result in a patient with no symptoms of an autoimmune disease may not be clinically significant. In such cases, the healthcare provider may choose to monitor the patient over time or repeat the ANA test at a later date.
Frequently Asked Questions About ANA Positive Results
Here are some common questions patients have about ANA positive results:
- What does it mean if my ANA is positive? A positive ANA means that antinuclear antibodies were detected in your blood. It doesn’t necessarily mean you have an autoimmune disease, but it warrants further investigation.
- What other tests will I need? Your doctor may order specific autoantibody tests, such as anti-dsDNA, anti-Ro/SSA, and anti-La/SSB, to help determine the underlying cause of your positive ANA. They may also order other blood tests, imaging studies, or biopsies.
- Will I need treatment? Treatment will depend on the underlying cause of your positive ANA. If you have an autoimmune disease, you may need medications to suppress your immune system and control your symptoms.
- Can a positive ANA go away? In some cases, a positive ANA can go away on its own, especially if it’s caused by a temporary factor, such as an infection or medication. However, if it’s caused by an autoimmune disease, it’s unlikely to go away completely.
- Is a high ANA titer always worse? Generally, a higher ANA titer suggests a higher likelihood of an autoimmune disease. However, the titer doesn’t always correlate with the severity of the disease.
- Can medications cause a positive ANA? Yes, certain medications can cause a drug-induced lupus, which can result in a positive ANA. Common culprits include hydralazine, procainamide, and isoniazid.
- I feel fine, but my ANA is positive. What should I do? If you feel fine but your ANA is positive, your doctor may choose to monitor you over time or repeat the test at a later date. It’s important to inform your doctor of any new symptoms that develop.
- Can stress cause a positive ANA? While stress can exacerbate symptoms of autoimmune diseases, it is not known to directly cause a positive ANA.
- Is there anything I can do to lower my ANA? There’s no specific way to lower your ANA level. Treatment focuses on managing the underlying condition causing the positive result.
- Should I be concerned about my children having a positive ANA? ANAs are not directly inherited. However, autoimmune diseases can have a genetic component. If you have an autoimmune disease, your children may have a slightly increased risk of developing one.
Empowering Understanding of ANA and ICD-10
Understanding the complexities surrounding “ANA positive ICD-10” is crucial for both patients and healthcare professionals. While a positive ANA result can be a source of concern, it’s important to remember that it’s just one piece of the puzzle. Accurate diagnosis and coding require a thorough evaluation of the patient’s medical history, clinical findings, and laboratory results. By working together, patients and healthcare providers can navigate this complex landscape and ensure that individuals receive the appropriate care and support. We encourage you to discuss any concerns about ANA positive results with your healthcare provider and to seek out reliable resources for further information.
